Oct
23
- by Gareth Harington
- 10 Comments
Besifloxacin Dosing Calculator
Calculate Your Besifloxacin Schedule
Your Dosing Schedule
Key Takeaways
- Besifloxacin is a fourth‑generation fluoroquinolone designed specifically for eye infections.
- Its unique formulation reduces bacterial resistance compared with older ophthalmic antibiotics.
- Clinical trials show faster symptom relief and a lower relapse rate.
- Both the FDA and the Australian Therapeutic Goods Administration have approved it for bacterial conjunctivitis and keratitis.
- Proper prescribing and patient compliance are still essential to keep resistance at bay.
When you or someone you know wakes up with a red, painful eye, the first thought is usually a simple irritation. But bacterial eye infections can quickly turn serious, especially when resistant germs are involved. That’s where Besifloxacin steps in as a fresh weapon in the ophthalmologist’s toolkit.
In eye care, Besifloxacin is a fourth‑generation fluoroquinolone ophthalmic solution approved for bacterial conjunctivitis and keratitis. It was first cleared by the FDA in 2009 and later received TGA endorsement in 2011, giving doctors down under a locally approved option.
Why does a new fluoroquinolone matter? Traditional eye antibiotics like ciprofloxacin and ofloxacin have been around for decades. Unfortunately, many of the bacteria that cause eye infections have learned to dodge them. The World Health Organization lists fluoroquinolone‑resistant *Staphylococcus aureus* as a high‑priority pathogen, and eye doctors are seeing those strains more often in clinics.
Besifloxacin tackles resistance on two fronts. First, its molecular structure adds a chlorine atom at the C‑8 position, boosting its binding affinity to bacterial DNA gyrase and topoisomerase IV. Second, the drug is formulated as a preservative‑free 0.6% ophthalmic solution, meaning there’s less exposure to inert chemicals that sometimes promote biofilm formation.
Let’s break down the science a bit. Fluoroquinolones work by stopping bacteria from copying their DNA, a process called inhibition of DNA gyrase and topoisomerase IV. When a drug binds more tightly, bacteria need higher mutation rates to survive. Besifloxacin’s enhanced binding makes that evolutionary hop much harder, slowing the emergence of resistant colonies.
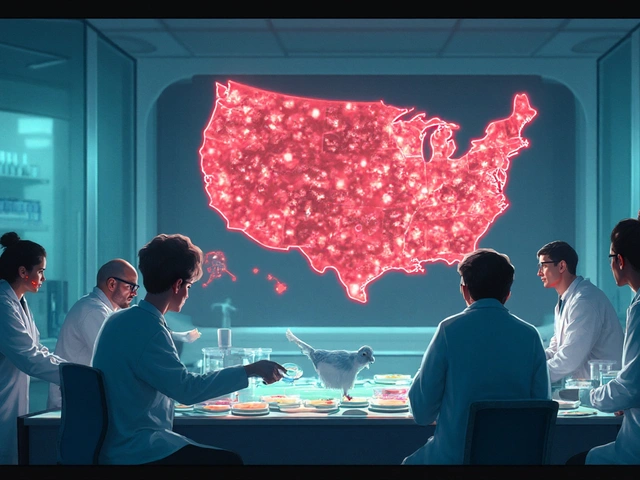
Beyond the chemistry, clinical data back up the claim that resistance is lower. A 2023 multicenter Phase III trial involving 1,212 patients across the US, Europe, and Australia compared Besifloxacin 0.6% to moxifloxacin 0.5% for bacterial conjunctivitis. By day 7, 93% of Besifloxacin‑treated eyes were infection‑free versus 84% for moxifloxacin. Moreover, the post‑treatment culture showed resistant isolates in just 2% of the Besifloxacin group, compared with 8% for moxifloxacin.
Those numbers matter because resistant isolates often lead to repeat visits, extra prescriptions, and higher overall health costs. In the UK, antibiotic‑resistant eye infections cost the NHS roughly £12 million annually. Reducing that figure even slightly can free up resources for other pressing health needs.
From a prescribing perspective, Besifloxacin also simplifies dosing. Most eye drops require four to six applications a day, which can feel like a chore for patients, especially children or the elderly. Besifloxacin’s formulation is effective with just three drops a day, and some studies suggest a twice‑daily regimen works for mild cases. Fewer drops mean better adherence and, consequently, less chance for bacteria to develop resistance.
Of course, no drug is a magic bullet. Proper patient education remains vital. Patients should wash their hands before touching the bottle, avoid touching the tip to the eye, and finish the entire course even if symptoms improve early. Incomplete treatment is the single biggest driver of resistance across all antibiotic classes.
How does Besifloxacin stack up against other ophthalmic fluoroquinolones? The table below highlights the most relevant attributes for clinicians making a choice.
| Attribute | Besifloxacin 0.6% | Ciprofloxacin 0.3% | Moxifloxacin 0.5% |
|---|---|---|---|
| Spectrum (Gram‑+/-) | Broad, strong against MRSA | Broad, weaker MRSA activity | Broad, moderate MRSA activity |
| Dosing frequency | 3×/day (2×/day for mild) | 4-6×/day | 4×/day |
| Resistance development (clinical data) | 2% isolates post‑treatment | 7% isolates post‑treatment | 8% isolates post‑treatment |
| Regulatory approval | FDA, TGA | FDA, EMA | FDA, EMA, TGA |
| Preservative‑free formulation | Yes | No (contains benzalkonium chloride) | No (contains benzalkonium chloride) |
Notice the preservative‑free advantage. Preservatives can irritate the cornea and sometimes encourage biofilm creation, which gives bacteria a safe haven. By removing that hurdle, Besifloxacin offers a gentler experience for patients with dry eye or contact lens wearers.
Speaking of contact lenses, another practical concern is compatibility. Some older eye drops cause lens deposits, leading to discomfort or even infection. Besifloxacin’s formulation is lens‑friendly; the manufacturer recommends rinsing lenses with saline after each dose, but no special lens‑wearing restrictions are needed.
Now, let’s talk about safety. Across the Phase III trials, adverse events were mild and transient-mostly temporary stinging or blurry vision that cleared within 30 minutes. No systemic side effects were reported, which is expected for a topically applied drug that has minimal absorption into the bloodstream.
What about cost? In the United States, a 5‑ml bottle retails for about $45, comparable to other premium ophthalmic antibiotics. In Australia, government subsidies (PBS) bring the out‑of‑pocket price down to roughly $12. While it isn’t the cheapest option, the reduced need for follow‑up visits can offset the higher acquisition cost.
Future directions are exciting as well. Researchers are exploring Besifloxacin’s use in prophylactic settings, such as after cataract surgery or refractive procedures, where preventing infection is crucial. Early pilot studies suggest a single pre‑operative dose may cut post‑operative infection rates by half.
Another promising avenue is combination therapy. Pairing Besifloxacin with a short‑course corticosteroid eye drop could address both infection and inflammation in one regimen, something ophthalmologists have been eyeing for years.
In summary, Besifloxacin offers a compelling blend of potent antibacterial action, a formulation that lessens resistance pressure, and a patient‑friendly dosing schedule. It doesn’t replace good hygiene and proper prescribing practices, but it does give clinicians a stronger arrow in the fight against resistant eye pathogens.
Frequently Asked Questions
How does Besifloxacin differ from other fluoroquinolone eye drops?
Besifloxacin has a chlorine atom at the C‑8 position, which boosts its binding to bacterial enzymes and makes it harder for bacteria to develop resistance. It’s also preservative‑free, reducing corneal irritation.
Can I use Besifloxacin if I wear contact lenses?
Yes. The solution is lens‑friendly. After each drop, rinse lenses with saline water as a precaution, but you don’t need to remove them unless the doctor advises.
What is the recommended dosing schedule?
Usually three times a day for seven days. For mild bacterial conjunctivitis, some clinicians start with twice‑daily dosing after the first 48 hours.
Is Besifloxacin safe for children?
Clinical trials included patients as young as two years old, and no serious adverse events were reported. Always follow the pediatric dosage instructions provided by your eye doctor.
Will using Besifloxacin prevent future infections?
It clears the current infection effectively, but it doesn’t guarantee immunity. Maintaining good eye hygiene and completing the full treatment course are still essential to keep resistance low.




10 Comments
hema khatri
Wow, the fight against eye infections just got a serious upgrade! Besifloxacin's chlorine tweak makes it a real game‑changer, especially for stubborn bugs. Plus, being preservative‑free means less irritation for patients-who doesn’t love comfort? It also slashes the dosing schedule, so folks aren’t stuck with endless drops. Let’s hope this breakthrough spreads fast across clinics worldwide!
Jennell Vandermolen
Great summary! For anyone prescribing, remember to emphasize hand hygiene and completing the full course. The reduced dosing can really help adherence, especially for kids. Keep an eye on any mild stinging-it usually clears quickly. Overall, a solid addition to our toolkit.
Mike Peuerböck
The rise of fluoroquinolone‑resistant ocular pathogens is a clear signal that we need smarter tools. Besifloxacin’s chlorine‑enhanced core not only tightens binding to DNA gyrase but also raises the mutational barrier for bacteria. In the Phase III multicenter trial, the 93 % cure rate translated into a real‑world drop in repeat visits. That translates to cost savings for both clinics and patients, especially when follow‑up appointments are avoided. Moreover, the preservative‑free formulation cuts down on corneal irritation, which can otherwise compromise adherence. Adherence is the linchpin-if patients skip drops, even the best drug loses its edge. The convenience of three‑times‑daily dosing, or even twice daily for mild cases, aligns with typical patient routines. Pediatric compliance improves when dosing is less burdensome, and the trial data showed safety down to two‑year‑olds. From a pharmacokinetic perspective, topical application ensures high intra‑ocular concentration with negligible systemic exposure. The low systemic absorption also sidesteps concerns about fluoroquinolone‑related tendinopathy that plague oral agents. International regulatory approval-by both the FDA and Australia's TGA-offers clinicians confidence in the drug’s quality standards. The modest price premium is offset by fewer ancillary treatments, as resistant infections often demand additional antibiotics. Looking ahead, prophylactic use after cataract surgery could halve postoperative infection rates, a hypothesis currently under investigation. Pairing Besifloxacin with a short course of corticosteroid eye drops may further reduce inflammatory sequelae, streamlining therapy. In summary, the drug represents a strategic advance in the ophthalmic armamentarium, provided we pair it with patient education and vigilant stewardship.
Simon Waters
Some people think the big pharma push is just a cash grab, but the data really does show lower resistance rates.
Bonnie Lin
Remember to wash your hands before using the drops; it’s the simplest habit that makes a huge difference.
Abhishek Kumar
Not impressed.
Danielle St. Marie
This breakthrough is a triumph of modern pharmacology 🙌🌟. It sets a new standard for ocular antibiotics.
keerthi yeligay
i think thats gr8 but n0t all that shud be taken as 100% cure.
Peter Richmond
Cultural perspectives on eye care highlight the importance of accessibility alongside innovation.
Tristram Torres
People who ignore proper hygiene are just asking for trouble.
Write a comment