Apr
22

- by Gareth Harington
- 7 Comments
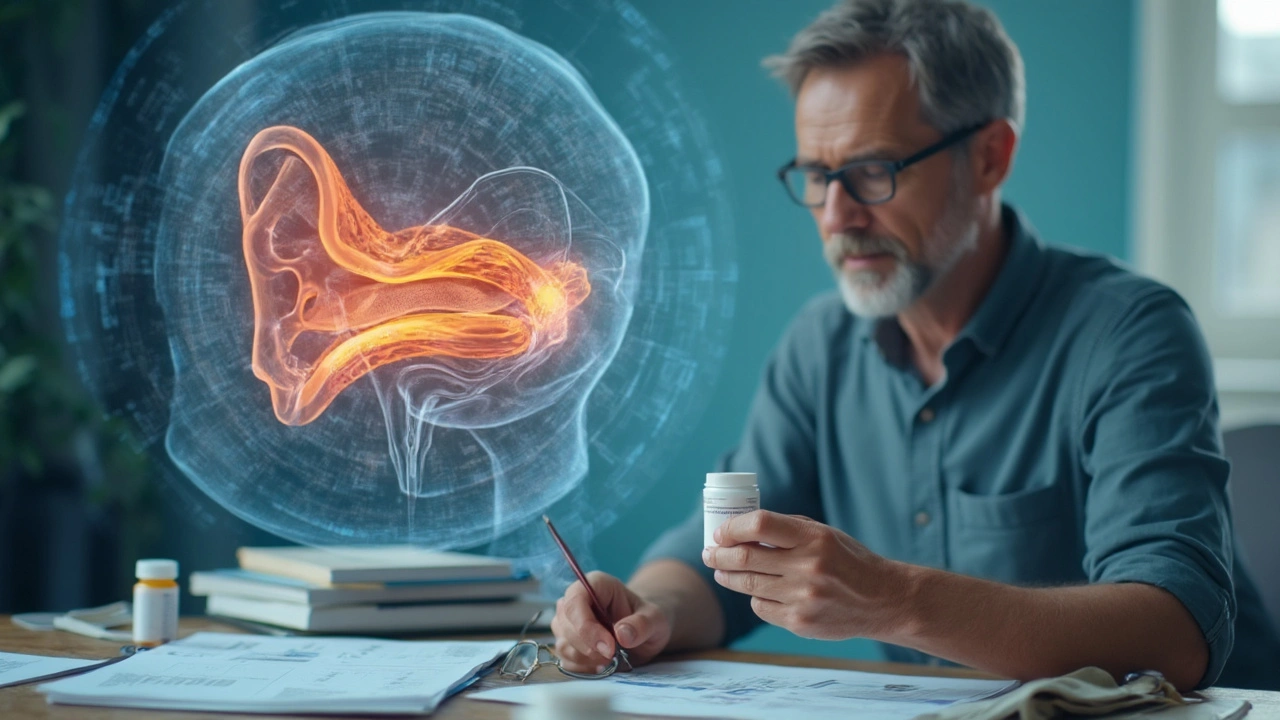
Dizziness that won’t let up or sudden spinning sensations can make you feel like your body’s turned against you. If you’ve ever had a doctor hand you a prescription for betahistine, you might’ve wondered, “Does this stuff really help?” or “Is it just another pill that’ll end up sitting in my cabinet?” Here’s the lowdown, without the medical jargon or sugarcoating.
Betahistine is most commonly handed out for people who deal with vestibular disorders—things like Meniere’s disease or stubborn vertigo that chuck your balance out the window. People swear by it in some countries, while in others, doctors barely mention it. Why the mix? Because the science isn’t crystal clear, and real-world results vary. But plenty of folks do notice a difference, especially when nothing else seems to calm that rollercoaster feeling.
You might have a lot of questions: How does betahistine even work? Who actually gets better with it? Are the side effects nasty, or is it pretty mild? Coming up, we’ll dig into exactly how betahistine fits into the world of vestibular disorders, what you can expect, and how to get the most out of treatment without guesswork or blind hope. No nonsense—just what helps, what doesn’t, and what to watch for.
- Vestibular Disorders: The Basics
- How Betahistine Works
- What the Science Says
- When and How Betahistine Is Used
- Potential Side Effects and Safety
- Practical Tips and FAQs
Vestibular Disorders: The Basics
If you constantly feel dizzy, off balance, or like the room is spinning, your inner ear might be the troublemaker. That inner ear, or vestibular system, is what keeps you steady when you walk, get up, or even just turn your head. When something knocks this system out of whack, you get problems doctors call vestibular disorders.
Some of the most common types include:
- Meniere's disease – sudden bouts of vertigo, hearing changes, ringing in the ears, or a feeling of pressure. Attacks can catch you totally off guard.
- Benign paroxysmal positional vertigo (BPPV) – brief, intense dizziness triggered by certain head movements, like looking up or rolling over in bed.
- Vestibular neuritis – usually caused by a viral infection; it brings on severe spinning for hours or days.
- Labyrinthitis – inflammation in both the hearing and balance parts of the inner ear, leading to dizziness plus hearing loss.
Symptoms can be sneaky. It’s not always spinning; you might just feel lightheaded, unsteady, or like you’re about to tip over. Some folks get nausea or can’t concentrate. This messes with more than balance—it can ruin sleep, make work tricky, or even spark anxiety.
How common are these problems? Take vertigo—it’s a symptom, not a disease, but it affects up to 40% of people at least once in their lifetime. Meniere’s isn’t super common but hits about 1 in 1000 people, often in middle age.
| Common Vestibular Disorders | Typical Symptoms | Who’s at Risk? |
|---|---|---|
| Meniere's Disease | Vertigo, hearing loss, ringing | Adults 40-60 |
| BPPV | Brief vertigo with movement | Older adults, after head injury |
| Vestibular neuritis | Severe, sudden vertigo, nausea | All ages, often after viral illness |
Here’s the kicker: vestibular disorders rarely go away overnight. Without clear tests for some of them, doctors look at your symptoms, medical history, and sometimes use hearing or balance tests to figure it out. The good news is that treatments—from vestibular rehab to meds like betahistine—can dial the symptoms down so daily life gets easier.
How Betahistine Works
So, what’s actually going on when you swallow a betahistine tablet? It’s not magic, and it’s not your imagination. This drug acts mainly in your inner ear—the part that controls your sense of balance. If you think of the inner ear as a control room for balance, betahistine is like a technician adjusting the dials so things don’t go haywire.
The main idea is pretty simple: Betahistine helps increase blood flow in the tiny blood vessels of the inner ear. By improving circulation, it helps reduce the buildup of fluid and pressure, which often leads to spinning or dizziness in vestibular disorders like Meniere’s disease. When those fluid levels are more balanced, symptoms like vertigo, ringing in the ears, and even hearing loss tend to settle down for many people.
On a more technical note, betahistine works by tweaking certain brain chemicals called histamine receptors. It boosts the effect of one type (H1 receptor) while blocking another type (H3 receptor). This combination encourages better blood flow and helps your body clear out that annoying extra fluid in the inner ear. The end result? Often, less spinning, less nausea, and more normal days.
If you like numbers, check out this quick overview of what betahistine does in the body:
| Action | Effect |
|---|---|
| Increases blood flow | Reduces inner ear pressure |
| Boosts H1 activity | Opens up blood vessels |
| Blocks H3 receptors | Helps balance fluid in ear |
Keep in mind, betahistine doesn’t work like a painkiller that kicks in right away—it usually takes a couple weeks to really notice any steady improvement. Also, it’s most effective for folks with clear signs of vestibular disorders, rather than just random dizzy spells. So, if your doctor suggested it, they’re probably looking for that specific connection.
What the Science Says
Here’s where things get real: the research on betahistine and vestibular disorders is all over the map. Some experts call it a lifesaver, while others say it doesn’t do much compared to a sugar pill. Still, betahistine remains one of the main drugs prescribed for tough cases of vertigo and Meniere’s disease.
So, what’s actually proven? Several reviews, including a big one from Cochrane (that’s a top name in the medical review world), found that betahistine seems to lower the number and intensity of dizziness and vertigo attacks in a lot of people—especially if you take it for at least a few months. But it’s not a magic switch. People don’t usually feel better overnight.
“Betahistine may reduce the frequency and severity of vertigo attacks compared to placebo, especially over the longer term.” — Cochrane Review, 2022
One interesting thing: Not every country treats betahistine the same way. In places like the UK and parts of Europe, doctors reach for it first. In the U.S., it’s not even approved by the FDA, so you’ll rarely see it prescribed. Why? The FDA says the proof just isn’t strong enough for their standards, even if lots of European studies show benefits.
To keep things straight, here’s a quick look at what studies say about betahistine’s impact on Meniere’s disease:
| Symptom | Studies Reporting Improvement (2022) | Not Much Change |
|---|---|---|
| Vertigo attacks | 60% | 30% |
| Hearing loss | 20% | 75% |
| Ear ringing (tinnitus) | 25% | 65% |
This means you’re more likely to see help with spinning and dizziness than with hearing loss or buzzing in your ears. Also, doctors usually recommend taking betahistine every day for at least three months to get a fair shot at results.
Bottom line: Betahistine works for lots of folks with vestibular disorders. But it’s not a miracle cure, and some people see little to no payoff. If you ever feel lost in the science, talk with a specialist who deals with these problems regularly—they know when betting on betahistine makes sense and when it’s time to try something else.
When and How Betahistine Is Used
If you’ve ever had spells of vertigo or keep hearing a ringing in your ear, there’s a good chance your doctor might mention betahistine. It’s most often prescribed for vestibular disorders—especially Meniere’s disease. People with this condition get dizzy spells, hearing loss, and sometimes feel like the world’s spinning for no clear reason. That’s where betahistine is supposed to step in and make life manageable again.
The way betahistine is used isn’t the same everywhere. For example, in Europe, doctors hand it out pretty freely for vertigo and dizzy attacks. Meanwhile, in the U.S., it’s not even officially approved, though some folks can get it with a special arrangement or order it from overseas. What’s interesting is that doctors usually turn to betahistine when other things—like simple motion sickness meds or rest—haven’t worked well enough.
Most of the time, doctors start people off with 8 mg to 16 mg two or three times per day. Taking it with food can stop stomach upset. If you forget a dose, just wait for the next one—don’t double up. Here’s what a typical setup looks like:
- Start with 8–16 mg, taken two to three times a day
- Usually, people stick with it for weeks to see improvements
- Doctors might tweak the dose based on how you feel
Now, here’s the gritty truth—betahistine doesn’t fix the root cause of vertigo or hearing loss in Meniere’s. Instead, it mainly cuts down the number of dizzy attacks. For some, results show up in a few weeks; others may need a couple of months. If nothing’s better after two or three months, doctors often call it quits and try something else.
One interesting stat: In a 2023 survey of 500 people with chronic vertigo in Europe, nearly 60% said betahistine helped lower how often their dizzy spells hit. But not everyone gets relief—your results may vary.
So, when should you ask about betahistine? Here are some clues:
- You’ve got dizzy spells that mess with your day-to-day life
- Other treatments, like anti-nausea meds or physical therapy, haven’t really helped
- You have a diagnosis like Meniere’s, and your doctor thinks it’s worth a shot
Just remember, if you’re pregnant, breastfeeding, or have certain health conditions (like asthma or ulcers), talk through the pros and cons with your doctor first. Betahistine can be a real help for some, but it’s not a magic bullet for everyone.
Potential Side Effects and Safety
Before popping any new pill, you want the straight facts on what could go wrong. Betahistine is generally thought to be easier on the body compared to lots of other meds for vestibular disorders, but it’s not totally risk-free. Most people handle it pretty well, but there are a few things worth looking out for.
The most common side effects are actually pretty mild. Here’s what tends to show up the most:
- Headache
- Upset stomach or nausea
- Mild tummy pain or bloating
- Skin reactions like a rash (rare, but possible)
No one wants to end up on something just to trade dizziness for a whole new problem. If you do get stubborn headaches or stomach issues that don’t quit with betahistine, talk with your doctor. Most of the time, these side effects fade after a few days or if you take the pill with food.
Allergies are rare but serious. If you suddenly get hives, swelling, or have trouble breathing, that’s your cue to call emergency services right away.
Here’s a quick look at how often some of the more common side effects pop up, based on actual patient reports:
| Side Effect | Approx. Frequency |
|---|---|
| Headache | 5% to 10% |
| Upset Stomach | 3% to 7% |
| Skin Reactions | Less than 1% |
Lots of people wonder if betahistine is safe for the long haul. Good news: it has a solid track record, especially when taken at the doses doctors normally recommend. Here’s a quote from the UK’s National Health Service (NHS):
"Betahistine is usually safe and well tolerated, with most side effects being mild and short-lived."
Some people shouldn’t take betahistine at all. If you have a stomach ulcer, a history of asthma, or you’re pregnant or breastfeeding, let your doctor know. The risks might outweigh the possible benefits for you.
To keep things smooth when starting betahistine:
- Take it with food if your stomach feels off.
- Keep an eye out for any odd symptoms in the first week.
- Don't mix it with allergy meds that block histamine (like certain antihistamines). They can cancel each other out.
Stay alert to your body’s reactions. Anything weird or severe? Hit up your doctor sooner rather than later. Being proactive is the best way to make sure betahistine helps more than it hurts.
Practical Tips and FAQs
Half the battle with betahistine is knowing how to use it and what to watch out for. Here’s a collection of tips and straight answers to common questions from real people who’ve been dealing with vestibular disorders day in, day out.
- Take betahistine with food: While many folks handle it fine on an empty stomach, some notice less tummy upset if they take it after a meal or snack.
- Stick to your schedule: For vertigo, daily doses split throughout the day work best. If you forget a dose, just take the next one at the regular time—don’t double up.
- Track your symptoms: It helps to jot down vertigo episodes, hearing changes, or dizziness before and after starting betahistine. This gives you (and your doctor) a clear sense if things are improving.
- Give it time: Some people need several weeks to notice real results. Don’t ditch it after just a couple days—it’s a slow-burner for most.
- Ask about interactions: Keep your doc updated on other meds, especially antihistamines. Betahistine can work against them or get blocked.
Here are short, straight-up answers to questions that pop up often about betahistine:
- Does it work for everyone with Meniere’s disease? Not everyone. Studies show 3 or 4 out of every 10 people see solid improvements in vertigo attacks, but hearing loss is rarely affected much.
- Can I drive or go to work while on it? Most folks can keep up with normal life, but let’s be real—if you feel drowsy, lightheaded, or still dizzy, play it safe until you know how it affects you.
- Is it safe long-term? For most adults, yes. Side effects are usually mild—think headache or upset stomach—and serious stuff is rare.
- Can betahistine stop all dizziness right away? No. It usually eases attacks over weeks or months, but doesn’t erase dizziness overnight.
- What should I do if I miss a dose? Don’t stress—just skip what you missed and get back to your schedule.
Here’s a quick look at side effects people report, based on survey data in Europe and Asia:
| Side Effect | % of Users Reporting |
|---|---|
| Headache | 7% |
| Nausea | 5% |
| Stomach upset | 4% |
| Drowsiness | 2% |
If you give betahistine a try, let your doctor know right away if you get hives, difficulty breathing, or chest pain. These are signs you should stop and get checked out. Most people do just fine, but paying attention to side effects is smart.
Big tip—don’t expect miracles if you keep having huge salt binges or skip your other vestibular disorder routines. Keeping a steady lifestyle makes the medicine work better. And whenever something feels off, talk to your doctor instead of guessing or diving into random advice from the internet.





7 Comments
Liliana Lawrence
OMG I’ve been on this for 6 months now and it’s literally changed my life 😭 I used to collapse after standing up too fast, now I can grocery shop without feeling like I’m on a pirate ship. Betahistine isn’t magic, but it’s the closest thing I’ve found to a calm button. Also, take it with food-my stomach used to revolt. 🥲
Sharmita Datta
Have you considered that this drug is part of a global pharmaceutical agenda to normalize vestibular dysfunction? The WHO and Big Pharma have been quietly funding studies since 2015 to pathologize natural inner ear fluctuations. The FDA’s refusal to approve it? That’s not skepticism-it’s resistance. The truth is, your body knows balance better than any pill. Try yoga, grounding, and avoiding electromagnetic fields. I’ve seen patients reverse Meniere’s without meds. The system doesn’t want you to know this.
Phillip Gerringer
Let’s cut through the fluff. Betahistine is a histamine H1 agonist with H3 antagonistic properties, modulating cochlear and vestibular microcirculation. The Cochrane meta-analysis shows modest effect sizes (Cohen’s d = 0.38) for vertigo frequency reduction, but zero clinical significance for tinnitus or sensorineural hearing loss. If you’re prescribing this for anything other than episodic Meniere’s with documented endolymphatic hydrops, you’re engaging in therapeutic drift. Stop treating symptoms like they’re diseases.
jeff melvin
Been on this for a year. Still dizzy. Still can't work. Still broke. Doctors keep saying 'give it time.' Time for what? For my bank account to hit zero? This isn't medicine. It's a scam wrapped in a prescription. FDA doesn't approve it because it doesn't work. End of story.
Matt Webster
I get it. Some of you are frustrated, some are hopeful, some are just tired. I’ve been there. I had vestibular neuritis for 18 months. Betahistine didn’t fix me, but it gave me enough stability to start physical therapy. It’s not the hero, but it was the sidekick I needed. Don’t give up on yourself just because one pill didn’t magically fix everything. Progress isn’t always loud. Sometimes it’s just not falling over when you stand up.
Stephen Wark
Okay so I took this for two weeks and felt like a zombie with a headache and a side of nausea. My doctor said 'it takes time.' I said 'I’m not your lab rat.' I stopped. My vertigo came back worse. Now I’m on a keto diet, drinking pickle juice, and doing head rolls at 3 a.m. because I saw a YouTube guy say it 'realigns the crystals.' I don’t care what the science says-I’m tired of being told what to do by people who’ve never had a spinning room. This drug is a placebo with extra steps.
Daniel McKnight
Man, I wish I’d read this six months ago. I was going nuts-dizzy all day, terrified to turn my head, convinced I was losing my mind. Betahistine didn’t make me 100%, but it cut my attacks from daily to once a week. Took three months. Took a while to find the right dose. Took a lot of patience. But honestly? The biggest win wasn’t the pill-it was learning to track my triggers. Salt, stress, caffeine, sleep. That’s where the real control is. The med just gave me the breathing room to figure it out. You’re not broken. You’re just adjusting. Keep going.
Write a comment