Oct
30

- by Gareth Harington
- 14 Comments
Many people take atorvastatin to lower their cholesterol, and some also take thiamine (vitamin B1) for energy, nerve health, or because their doctor recommended it. But what happens when you take them together? Is it safe? Could one affect the other? These are real questions people ask when they’re managing multiple supplements and prescriptions.
What is atorvastatin?
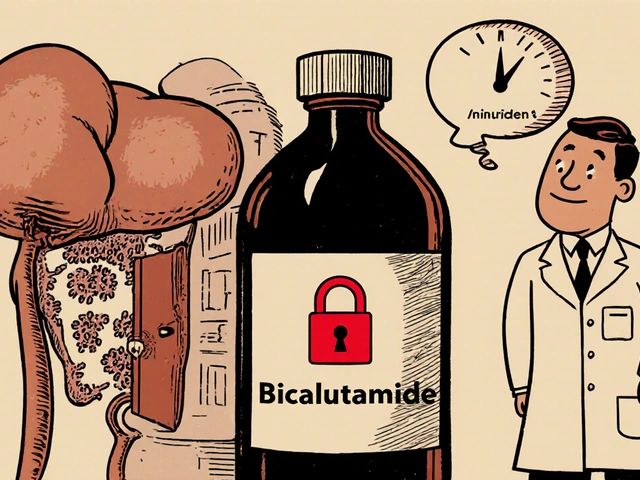
Atorvastatin is a statin medication used to reduce LDL (bad) cholesterol and triglycerides in the blood. It works by blocking an enzyme in the liver that makes cholesterol. Common brand names include Lipitor and generic versions sold worldwide. It’s prescribed for people with high cholesterol, heart disease risk, or type 2 diabetes. Most people take it once daily, often in the evening.
Side effects are usually mild-muscle aches, stomach upset, or headaches-but in rare cases, it can cause serious muscle damage (rhabdomyolysis) or liver issues. Blood tests are often done to monitor liver enzymes and muscle markers, especially when starting or increasing the dose.
What is thiamine?
Thiamine, or vitamin B1, is a water-soluble vitamin your body needs to turn food into energy. It’s critical for nerve function, heart health, and brain activity. You get it from whole grains, meat, fish, beans, and fortified cereals. Most people don’t need supplements because they get enough from diet.
But certain groups do-people with alcohol use disorder, those with malabsorption conditions like Crohn’s disease, diabetics, and older adults. Thiamine deficiency can lead to beriberi (affecting nerves and heart) or Wernicke-Korsakoff syndrome (a brain disorder). Supplements come in pills, injections, or as part of B-complex vitamins.
Do atorvastatin and thiamine interact?
There’s no known direct chemical interaction between atorvastatin and thiamine. That means thiamine doesn’t stop atorvastatin from working, and atorvastatin doesn’t break down thiamine faster or slower.
Major drug databases like Micromedex, Lexicomp, and the FDA’s labeling for Lipitor don’t list thiamine as a concern. The same goes for clinical guidelines from the American Heart Association and the European Society of Cardiology.
So, on paper, it’s safe to take them together. But safety isn’t just about chemistry-it’s about what’s happening in your body.
Indirect effects: What your body might be telling you
Even without a direct interaction, there are indirect ways these two can affect each other’s impact.
First, atorvastatin can slightly raise blood sugar levels. That’s why doctors monitor HbA1c in people with prediabetes or diabetes. Thiamine, on the other hand, plays a role in insulin sensitivity. Some small studies suggest thiamine supplements might help improve glucose metabolism in diabetics. So if you’re taking both, your blood sugar could respond differently than expected-especially if you’re already managing diabetes.
Second, muscle pain is a common complaint with statins. Thiamine deficiency can also cause muscle weakness and cramps. If you’re taking atorvastatin and suddenly feel more tired or achy, it’s possible you’re low in thiamine-not because the drug is causing it, but because your body’s demands changed. Alcohol use, poor diet, or chronic illness can drain thiamine stores, and statins don’t help refill them.
Third, liver health matters. Atorvastatin is processed by the liver. Thiamine supports liver function by helping break down carbohydrates and reducing oxidative stress. If your liver is already under strain from other factors (alcohol, fatty liver, medications), having enough thiamine could help it cope better. But thiamine won’t fix damage caused by statins-it just supports overall function.

Who should be extra careful?
Some people need to pay closer attention when taking both:
- People with diabetes: Monitor blood sugar closely. Thiamine might improve insulin response, which could mean your diabetes meds need adjusting.
- Heavy drinkers or recovering alcoholics: You’re likely low in thiamine. Atorvastatin won’t fix that. You may need higher-dose thiamine (100-300 mg/day) under medical supervision.
- Older adults: Appetite and nutrient absorption decline with age. A B-complex with thiamine might help more than just one vitamin.
- Those with muscle pain on statins: If your pain doesn’t improve after a few weeks, ask your doctor about checking thiamine levels. Low B1 can mimic statin side effects.
How to take them safely
If your doctor or pharmacist says it’s okay to take both, here’s how to do it right:
- Take atorvastatin at the same time every day. Evening is common, but consistency matters more than timing.
- Take thiamine with food. It’s better absorbed and less likely to cause stomach upset.
- Don’t assume all B-vitamins are the same. Some B-complex supplements contain high doses of niacin (B3), which can raise liver enzymes. Stick to plain thiamine or low-dose B-complex unless directed otherwise.
- Watch for new symptoms. Unexplained fatigue, tingling in hands or feet, confusion, or worsening muscle pain? Tell your doctor. These aren’t normal.
- Get blood tests if needed. A simple serum thiamine test isn’t routine, but if you’re at risk, ask for it. Liver enzymes (ALT, AST) and CK (creatine kinase) should be checked periodically on statins.
What if you miss a dose?
Missing one dose of atorvastatin won’t ruin your cholesterol control, but don’t double up the next day. Just take your regular dose when you remember.
Missing thiamine once? No big deal. It’s water-soluble, so your body flushes out what it doesn’t use. But if you’re taking it for a medical reason-like alcohol recovery or neuropathy-try not to skip regularly. Consistency helps your nerves and energy levels stay stable.
When to call your doctor
You don’t need to panic over every little change. But call your provider if you notice:
- Severe muscle pain or weakness, especially with dark urine
- Unusual tiredness, confusion, or memory problems
- Swelling in your legs or rapid heartbeat
- Yellowing of skin or eyes (sign of liver stress)
- Any new symptoms that started after adding thiamine
These aren’t common, but they’re serious. Don’t wait. Your doctor might adjust your statin dose, check your thiamine levels, or run other tests.
Real-life example: Mary’s story
Mary, 68, was on atorvastatin for high cholesterol. She also started taking a thiamine supplement after her doctor said she was borderline deficient. Within two weeks, her muscle aches got worse. She thought it was the statin. But when she got her blood work done, her thiamine level was still low. Her doctor increased her thiamine dose to 200 mg daily. Within three weeks, her muscle pain improved. Her cholesterol stayed controlled. She didn’t stop the statin-she just fixed the missing vitamin.
That’s the point: sometimes what looks like a drug side effect is really a nutrient gap.
Bottom line
Atorvastatin and thiamine can be taken together safely. There’s no dangerous interaction. But they’re not just pills-they’re tools that affect how your body works. If you’re taking both, pay attention to how you feel. Don’t assume everything is normal just because the drugs don’t "officially" conflict.
Low thiamine can hide behind statin side effects. High blood sugar might shift with added B1. Your liver needs support. Your nerves need fuel.
Talk to your doctor. Get tested if you’re at risk. Don’t guess. Your health isn’t about avoiding interactions-it’s about making sure every piece of your treatment plan works together.
Can I take thiamine with atorvastatin?
Yes, you can safely take thiamine with atorvastatin. There is no known direct drug interaction between them. Thiamine does not interfere with how atorvastatin lowers cholesterol, and atorvastatin does not reduce thiamine levels in your body.
Does atorvastatin cause thiamine deficiency?
No, atorvastatin does not cause thiamine deficiency. However, people who take statins often have other risk factors for low thiamine-like diabetes, poor diet, alcohol use, or aging. These conditions, not the statin itself, are more likely to lower thiamine levels.
Can thiamine help with statin muscle pain?
In some cases, yes. Thiamine deficiency can cause muscle weakness and cramps that feel similar to statin side effects. If you have low thiamine levels, correcting it may reduce muscle discomfort. But if your pain is from statin-induced muscle damage, thiamine won’t fix it. Always check your levels before assuming it’s a vitamin issue.
Should I take thiamine if I’m on atorvastatin?
Only if you need it. Most people get enough thiamine from food. But if you’re diabetic, drink alcohol regularly, are over 65, or have digestive issues, your doctor might recommend a supplement. Don’t take it just because you’re on a statin-take it because your body needs it.
How long does it take for thiamine to work?
If you’re deficient, you might feel better in a few days-especially in energy levels and nerve symptoms. Muscle improvements can take 2-4 weeks. For serious deficiencies (like in alcoholism), doctors often give high-dose injections first, then switch to oral supplements.





14 Comments
Casey Crowell
Man, I was just telling my buddy this last week-he’s on Lipitor and started taking B1 because his legs were cramping like crazy. Thought it was the statin, turns out he’s been low as hell on thiamine since his diabetes diagnosis. Two weeks of 200mg and he’s hiking again. Who knew? 🙌
Shanna Talley
This is the kind of post that actually helps. So many people panic when they add a supplement without knowing why. Thiamine isn’t magic but it’s way more important than most realize. If you’re tired, achy, or fuzzy-headed-check your B1. It’s cheaper than a doctor’s visit and way safer than guessing. 💪
Samuel Wood
Look i dont know why people are making this so complicated. Statins and B1? Obviously no interaction. I mean come on its basic biochemistry. If you think your muscles hurt because of the statin you probably just dont like taking pills. Also why are you even on a statin if you dont eat meat? 🤷♂️
ridar aeen
Samuel, you’re missing the point. It’s not about whether they interact chemically-it’s about how your body *feels*. I had chronic fatigue for years. Took B1 on a whim. Three days later I could walk up stairs without stopping. Atorvastatin? Still taking it. But now I’m not just surviving. I’m living. 🤍
chantall meyer
Most people taking statins are obese, sedentary, and eat nothing but processed carbs. Of course they’re deficient in thiamine. It’s not the drug-it’s their lifestyle. Fix the root cause before popping pills. Also, if you’re taking supplements without a blood test, you’re not healthcare-you’re gambling.
Jacqueline Anwar
While I appreciate the attempt at clarity, this post lacks sufficient citation of peer-reviewed clinical trials. The anecdotal reference to Mary’s case is not evidence-based medicine. Furthermore, the suggestion that thiamine supplementation may modulate insulin sensitivity requires rigorous double-blind studies before being generalized to diabetic populations. This is dangerously close to nutritional pseudoscience.
Ganesh Kamble
lol atorvastatin and thiamine? bro just stop taking both. you dont need either. eat less sugar, move more, stop being a hypochondriac. everyone’s on pills these days like its a trend. i’ve never taken a vitamin and my cholesterol’s fine. you’re overcomplicating life.
Jenni Waugh
Let me get this straight-you’re telling people to take a vitamin because their statin side effects might be misdiagnosed? And you’re not even mentioning that thiamine is sold in 500mg doses on Amazon by a guy named "Dr. Miracle" who lives in a van? 🙄 This isn’t medicine-it’s influencer content with a lab coat. Also, if your liver’s stressed, maybe stop drinking wine at 5pm?
Theresa Ordonda
People are dying because they think vitamins fix everything. Statin myopathy is real. Thiamine deficiency is real. But throwing B1 at every ache isn’t healing-it’s distraction. If you’re not getting blood work done before and after, you’re not managing your health-you’re performing a ritual. 🩸
Judy Schumacher
Let’s be honest: the entire premise of this post is built on the assumption that the average person can interpret lab results, understand pharmacokinetics, and self-diagnose nutrient deficiencies without professional oversight. This is not empowerment. This is medical malpractice dressed up as wellness. And Mary’s story? That’s not a case study-it’s a cautionary tale about confirmation bias. You don’t fix statin-induced rhabdomyolysis with a vitamin. You stop the statin. Period.
Megan Raines
Wait so if I take B1 and my muscle pain goes away… does that mean it was never the statin? Or does it mean the statin made me deficient? And if so, why don’t doctors test for this before prescribing? …I’m just asking.
Mamadou Seck
Y’all are overthinking this. I take both. I drink coffee, eat tacos, and still live. If your body’s falling apart maybe try sleeping more instead of chasing vitamins like they’re magic beans. Also thiamine? Sounds like a character from a fantasy game. 🧙♂️
Anthony Griek
I’ve been on atorvastatin for 8 years. Started thiamine last year after my neurologist mentioned it. My feet stopped tingling. My brain fog lifted. No drama. No miracle. Just a simple fix for a simple gap. I’m not a biochemist. I’m just someone who listens to their body. And yeah, I get blood work every 6 months. No biggie.
Norman Rexford
Look I’m all for vitamins but this is why America’s falling apart. We’re not supposed to need supplements. Back in my day we ate real food, worked in the yard, and didn’t take pills for everything. Now everyone’s got a B1 regimen because they sat on their butt all day eating Pop-Tarts. Fix your damn diet. And if you’re drinking and taking statins? You’re asking for trouble. 🇺🇸
Write a comment